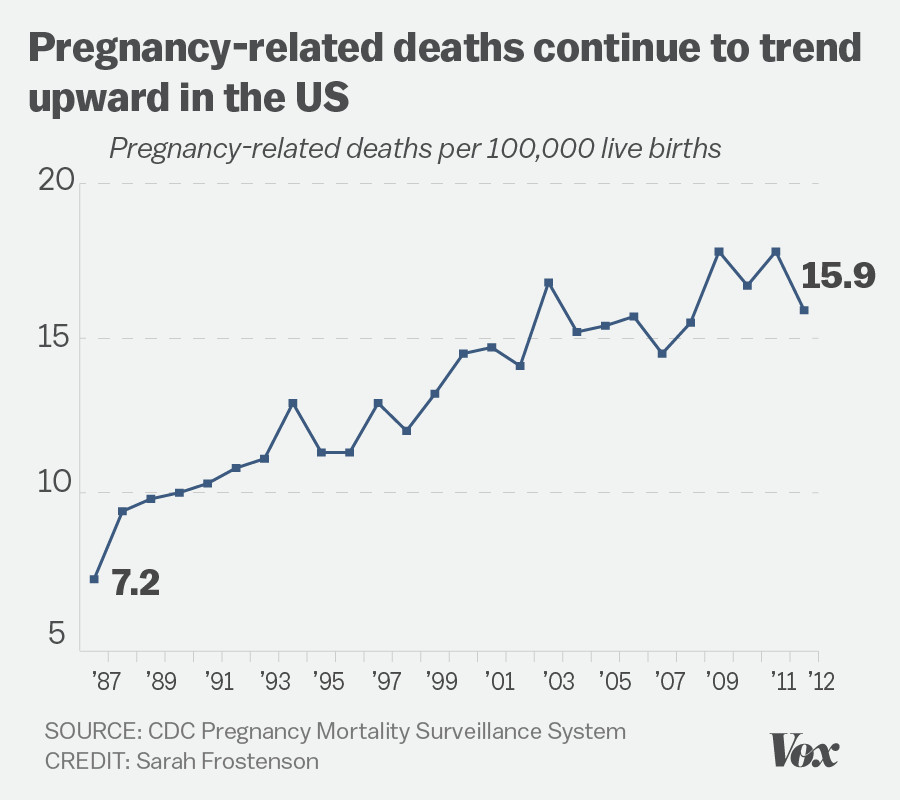
Pregnancy-related deaths have become a pressing public health crisis in the United States, where the maternal mortality rate has been persistently high compared to its peers among affluent nations. Alarmingly, over 80% of these fatalities are deemed preventable, highlighting the urgent need for improved maternity care. A recent study revealed a continuous rise in pregnancy-related deaths between 2018 and 2022, particularly affecting marginalized communities due to healthcare disparities. With chronic health conditions, such as cardiovascular disease, becoming a leading cause of these tragic outcomes, it is imperative to address systemic issues in prenatal and postpartum care. By prioritizing comprehensive healthcare strategies and interventions, we can significantly reduce preventable deaths during pregnancy and improve maternal health for future generations.
Addressing the challenge of maternal health in the U.S. calls for a thorough examination of the rising incidence of death associated with pregnancy and childbirth. This sobering issue, often referred to as maternal mortality, not only highlights the preventable nature of many associated fatalities but also underscores the differences in health outcomes based on varying demographics. The alarming trend of increased mortality rates among certain racial and ethnic groups emphasizes the urgent need for targeted solutions. Furthermore, the significant role that chronic health issues play in adverse pregnancy outcomes cannot be overlooked. By fostering comprehensive and equitable postpartum care and addressing the complex intersection of health disparities, we can pave the way for safer pregnancies and healthier mothers.
Understanding Maternal Mortality in the U.S.
Maternal mortality, defined as the death of a woman during pregnancy or within 42 days of giving birth, represents a significant public health issue in the United States. Alarmingly, recent studies indicate that the U.S. stands out among high-income countries with the highest rates of maternal mortality. This statistic is particularly troubling considering that over 80% of these pregnancy-related deaths are preventable, suggesting that there is a critical need for improved healthcare systems and policies. To address maternal mortality effectively, it is essential to identify the multifaceted factors contributing to these deaths, including access to quality prenatal care, healthcare disparities across racial and ethnic lines, and the rising prevalence of chronic health conditions among pregnant individuals.
In recent years, there has been a stark rise in maternal mortality rates, especially during the period influenced by the COVID-19 pandemic. The findings from the National Institutes of Health (NIH) underscore this concerning trend, revealing that certain demographics, particularly American Indian and Alaska Native women, have disproportionately higher rates of pregnancy-related deaths. Understanding these disparities is vital to developing targeted interventions that address the underlying causes of maternal mortality in various communities.
To comprehend the landscape of maternal mortality in the U.S., it is vital to consider the role of systemic healthcare disparities. Research indicates that geographic location plays a critical role in maternal health outcomes, with certain states reporting significantly higher rates of maternal mortality. The significant variability across state lines points to the necessity for comprehensive policy changes and improved healthcare access to ensure equitable care. Furthermore, chronic conditions such as hypertension and diabetes can complicate pregnancy and postpartum recovery, leading to increased risk of serious health complications or death. Hence, addressing these chronic health issues through better prenatal care can contribute significantly to reducing maternal mortality rates.
Preventable Deaths During Pregnancy: A Call for Action
The staggering statistic revealing that over 80% of pregnancy-related deaths in the U.S. are preventable serves as a wake-up call to healthcare policymakers and providers. These preventable deaths are often the result of inadequate prenatal and postpartum care, which can be addressed through implementing comprehensive healthcare reforms. Investing in accessible pregnancy care, enhancing the skills and training of healthcare providers, and ensuring equitable healthcare access for all women are essential steps to mitigate this preventable crisis. Furthermore, education regarding maternal health risks and the management of chronic conditions can significantly contribute to better outcomes for pregnant individuals and their infants.
Additionally, the importance of continuous postpartum care cannot be overstated. The findings that a significant proportion of maternal deaths occur after childbirth, within the first year, highlight the necessity for ongoing healthcare access. Women must be supported with resources and care throughout their entire postpartum period, rather than solely within the first few weeks after delivery. By addressing these critical gaps in care, stakeholders can work towards significantly reducing preventable pregnancy-related deaths.
Enhancing community awareness around maternal health can catalyze support for policies that prioritize the health and well-being of women during pregnancy and the postpartum period. Programs that promote maternal education, support networks, and access to professional healthcare guidance are vital in combating preventable deaths during pregnancy. Furthermore, creating awareness regarding the signs and symptoms of serious postpartum complications can empower women to seek timely medical attention, significantly decreasing the risk of preventable maternal deaths. Engaging local communities in maternal health initiatives can foster a more supportive and understanding environment that celebrates and prioritizes women’s health.
Healthcare Disparities and Their Impact on Maternal Health
The significant discrepancies in maternal mortality rates among various demographic groups in the U.S., particularly along racial lines, highlight the enduring issue of healthcare disparities. Studies indicate that women from marginalized communities, including American Indian and Alaska Native, as well as non-Hispanic Black women, face disproportionately high rates of pregnancy-related deaths compared to their white counterparts. This inequity underscores the urgent need for targeted healthcare policies that address the systemic biases and barriers that these women encounter within the healthcare system. Understanding the root causes of these disparities is crucial to developing effective interventions aimed at improving maternal health outcomes for all women, regardless of their background.
Furthermore, the lack of access to quality prenatal and postpartum care for minority women is often exacerbated by social determinants of health, including socioeconomic status, education, and geographic location. Addressing these root causes requires collaborative efforts from healthcare stakeholders, policymakers, and community organizations to dismantle the barriers that prevent at-risk populations from receiving the care they need. This can include initiatives aimed at increasing the diversity of healthcare providers, providing culturally competent care, and improving healthcare access in underserved areas. Through strategic collaboration and advocacy, we can begin to bridge the healthcare gaps that contribute to maternal mortality discrepancies.
Increasing awareness of healthcare disparities surrounding maternal health must be a collective effort involving communities, healthcare providers, and policymakers. It’s essential to foster discussions that encompass the lived experiences of women from various backgrounds who encounter these disparities. By actively involving these communities in the conversation, stakeholders can develop targeted solutions that are not only effective but also culturally relevant. Initiatives such as community health workshops, targeted outreach for maternal health services, and providing resources that address the unique challenges faced by diverse populations can help mitigate the adverse effects of healthcare disparities on maternal mortality.
As we aim for more equitable maternal health outcomes, it’s critical to monitor the effectiveness of implemented strategies continuously. Creating systems for feedback and assessment will ensure that interventions resonate with the community’s needs and adapt to changing demographic landscapes. This multifaceted approach empowers women and communities while contributing to a gradual but necessary shift in maternal health equity.
The Role of Chronic Health Conditions in Pregnancy-Related Deaths
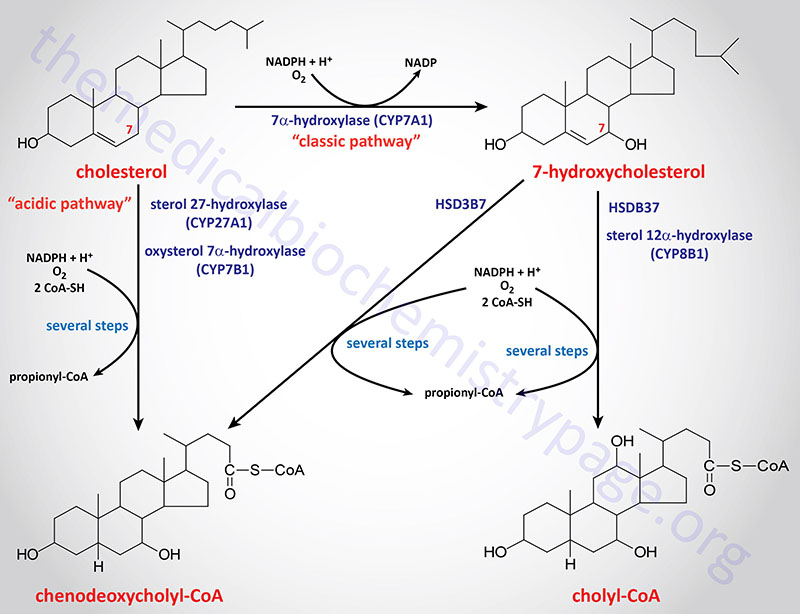
Chronic health conditions have been identified as a significant factor contributing to pregnancy-related deaths in the U.S., with cardiovascular disease emerging as the leading cause of maternal mortality. As the population of women of reproductive age faces a rising prevalence of conditions such as hypertension, diabetes, and obesity, the implications for maternal health become increasingly concerning. Medical professionals must prioritize the management of these chronic conditions during preconception and prenatal care, as effective interventions can greatly reduce risks associated with pregnancy complications. Encouragingly, awareness of the need for integrated healthcare models—where obstetricians collaborate with primary care providers to address chronic health issues—is growing among healthcare professionals.
To tackle the complexities introduced by chronic health conditions, healthcare systems need to establish protocols that ensure early identification and management of these risks. This can involve routine screening for chronic diseases during prenatal visits, as well as educational programs aimed at helping women understand how their existing health conditions may impact their pregnancies. Additionally, partnerships between healthcare providers and community resources can offer sustained support for women throughout their pregnancy and postpartum period, ultimately contributing to improved maternal health outcomes.
Addressing chronic health conditions in the context of maternal care also requires a deeper understanding of how these ailments evolve over time. As mentioned in the study, younger women are increasingly presenting with chronic conditions like hypertension that were traditionally seen in older populations. This shift necessitates a reevaluation of how healthcare is delivered to pregnant women, ensuring that services are tailored to address the unique needs of younger populations. Moreover, recognizing the interconnectedness of maternal health and chronic health management can lead to more comprehensive care models that enable better health outcomes for mothers and their newborns. This holistic approach not only benefits individual patients but can also alleviate systemic pressures on maternity care services by promoting healthier pregnancies.
Postpartum Care: Addressing the Critical Transition
Postpartum care is a vital aspect of maternal health that has historically received insufficient attention. Recent findings underscore the fact that a substantial proportion of pregnancy-related deaths occur during the postpartum period, highlighting two crucial aspects: the need for extended care beyond the immediate six-week postpartum visit and the importance of systems that effectively support women during their recovery. Current perceptions within the healthcare system often treat postpartum recovery as a rapid process, but the reality is that many women need ongoing support to address both physical and emotional health challenges. A shift in this mindset is essential to foster a more supportive framework for maternal health.
Engaging with healthcare providers to establish more comprehensive postpartum care can significantly impact health outcomes. Women should have access to resources that allow them to receive regular check-ups and ongoing consultations to monitor their recovery process. This includes addressing issues such as mental health, chronic pain, and other complications that arise after childbirth. Coupled with legislative changes to prioritize postpartum care as a fundamental part of maternal health, a more effective support system can emerge that not only reduces the risks of late maternal deaths but also promotes overall health and wellness for mothers.
Furthermore, healthcare systems must integrate postpartum care seamlessly into existing maternal health frameworks. This includes training providers to recognize and respond to potential postpartum complications and placing a stronger emphasis on educating new mothers about the signs of complications during their recovery. Community support systems and peer-to-peer programs can also play a crucial role in bridging gaps between professional care and personal lived experiences. By normalizing discussions around postpartum health, we create an environment where women feel empowered to seek help when needed and receive the comprehensive care that is essential for a healthy transition into motherhood.
Innovative Solutions to Enhance Maternal Health
As the challenges surrounding maternal mortality persist, innovative solutions must become a cornerstone of healthcare strategies aimed at enhancing maternal health outcomes. One promising approach is the integration of technology in prenatal and postpartum care. Digital health solutions, such as telemedicine platforms, mobile health applications, and remote monitoring tools, can provide women with greater accessibility to healthcare professionals and critical resources. This is especially vital for those living in rural areas or underserved communities, where access to healthcare can be limited. By leveraging technology, healthcare providers can maintain continuous communication with pregnant individuals, ensuring timely interventions and support.
Additionally, community-based initiatives are essential in fostering environments that support maternal health. These initiatives can take various forms, including educational programs that inform women about healthy pregnancy practices, partnerships with local organizations to provide resources tailored to specific communities, and campaigns that raise awareness about maternal health issues. In integrating these community-driven solutions with clinical care, stakeholders can create a holistic approach that not only addresses immediate healthcare needs but also builds long-term support systems for mothers throughout their maternity journey.
Another innovative solution lies in policy reforms aimed at increasing funding for maternal health research and programs. Investing in research will facilitate the collection of data necessary for understanding the complexities of maternal health and the factors contributing to maternal mortality. By focusing on preventative measures, states can better allocate resources towards initiatives that have proven effective in reducing maternal death rates. These initiatives may include expanding Medicaid coverage for postpartum care, implementing paid family leave policies, and developing comprehensive maternal health programs that involve a broad range of stakeholders, from healthcare professionals to community advocates. Only through collaborative and innovative efforts can we hope to achieve substantial improvements in maternal health outcomes.
Frequently Asked Questions
What are the main causes of pregnancy-related deaths in the U.S.?
Pregnancy-related deaths in the U.S. are primarily caused by chronic health conditions, particularly cardiovascular diseases, which account for over 20% of these deaths. Other significant factors include hemorrhage and the impact of healthcare disparities affecting maternal mortality, especially among minority populations.
How can healthcare disparities contribute to pregnancy-related deaths?
Healthcare disparities can lead to differences in access to quality care, preventive measures, and appropriate postpartum care, which exacerbate maternal mortality rates. Many pregnancy-related deaths are preventable, highlighting the need for equitable healthcare policies and support systems for all pregnant individuals.
What role does postpartum care play in preventing pregnancy-related deaths?
Postpartum care is crucial for preventing pregnancy-related deaths, as nearly a third occur between 42 days and one year after pregnancy. Comprehensive postpartum care can identify and manage chronic health conditions, ensuring mothers have the support necessary for healthy recovery after childbirth.
What are the statistics on preventable deaths during pregnancy in the U.S.?
In the U.S., more than 80% of pregnancy-related deaths are considered preventable. This alarming statistic underscores the critical need for improved healthcare policies and practices to reduce maternal mortality rates across diverse populations.
How does maternal mortality vary among different racial groups?
Maternal mortality rates show significant disparities among racial groups in the U.S. For example, American Indian and Alaska Native women experience mortality rates nearly four times higher than their white counterparts. These disparities emphasize the need for targeted strategies to address systemic inequities in maternal healthcare.
What strategies can be implemented to reduce pregnancy-related deaths?
To reduce pregnancy-related deaths, a multifaceted approach is needed, including enhancing access to prenatal and postpartum care, addressing healthcare disparities, investing in public health infrastructure, and implementing policies that provide comprehensive support for mothers throughout and after their pregnancies.
Why is there a need for better tracking of pregnancy-related deaths?
Improving the tracking of pregnancy-related deaths is essential for understanding the true scope of maternal mortality in the U.S. Since the national system was only established in 2018, consistent data collection can inform effective policy and guide interventions aimed at reducing preventable deaths during pregnancy.
How can chronic health conditions increase risks during pregnancy?
Chronic health conditions, such as hypertension and diabetes, can complicate pregnancies and increase the risk of pregnancy-related deaths. Addressing these issues early in reproductive-aged individuals is vital for reducing maternal mortality rates and ensuring healthier pregnancies.
What impact did the COVID-19 pandemic have on pregnancy-related deaths?
The COVID-19 pandemic has led to an increase in pregnancy-related deaths, peaking sharply in 2021. The pandemic has exacerbated existing healthcare challenges and disparities, affecting pregnant individuals’ care access and overall health outcomes.
What is the significance of late maternal deaths in the context of pregnancy-related mortality?
Late maternal deaths, occurring between 42 days and one year postpartum, account for a significant portion of pregnancy-related deaths. Recognizing these deaths highlights the importance of ongoing care and support for mothers well beyond the immediate postpartum period, advocating for a holistic approach to maternal health.
| Key Point | Details |
|---|---|
| Rising Pregnancy-Related Deaths | The U.S. has the highest maternal mortality rate among high-income countries. Rates increased from 25.3 deaths per 100,000 live births in 2018 to 32.6 in 2022. |
| Preventable Deaths | Over 80% of pregnancy-related deaths are preventable with better healthcare access and policies. |
| Racial Disparities | Significant disparities exist based on race; American Indian and Alaska Native women have the highest rates at 106.3 deaths per 100,000 live births. |
| Importance of Extended Postpartum Care | Late maternal deaths account for nearly 30% of pregnancy-related deaths, emphasizing the need for care beyond 42 days postpartum. |
| Need for Policy Changes | Investments in public health infrastructure and addressing state disparities are crucial to reduce mortality rates. |
Summary
Pregnancy-related deaths continue to be a significant concern in the United States, where the maternal mortality rate is notably higher than in other high-income nations. Over the years, increasing rates coupled with stark racial and geographic disparities highlight the urgent need for comprehensive healthcare reforms. As over 80% of these deaths are preventable, there is a pressing call for improved prenatal and postpartum care, targeted health policies, and enhanced public health infrastructure to address these challenges effectively.